Welcome to the ECHO Connector! The Environmental influences on Child Health Outcomes (ECHO) Program is a research program at the NIH with the mission to enhance the health of children for generations to come. The ECHO Connector will keep you informed of program news and our latest research findings.
Message from Matt
A message from the ECHO Director, Matthew W. Gillman, MD

September is National Childhood Obesity Awareness Month. Childhood obesity or overweight affects around 35% of children in the U.S., increasing their risk for adverse mental and physical health outcomes that can follow them into adulthood. Obesity is one of ECHO’s five pediatric health outcomes, and advancing research in the early developmental causes of obesity and its consequences is an important part of our mission to enhance the health of children for generations to come.
In this issue of the ECHO Connector, we will highlight the work of ECHO investigators including Drs. Traci Bekelman and Dana Dabelea, who have led a team of ECHO researchers in studying the regional and socioeconomic differences in childhood obesity. This team is also leading ECHO collaborative research on how obesity-related behaviors have changed with the COVID-19 pandemic, during which the already high rates of childhood obesity have risen even more. See below for more detail on their research.
ECHO's five pediatric health outcome areas

You can find more papers from ECHO researchers on obesity and other outcome areas on our publications page, which is searchable by topic.
I would also like to thank the ECHO Connector readers and ECHO participants for the feedback we have received thus far on the ECHO Connector and ECHOchildren.org website survey. We appreciate your participation and feedback and encourage you to complete the survey to help enhance ECHO’s communications and resources.

—Matthew W. Gillman, M.D., S.M.
Back to top![]()
ECHO Program Spotlight:
Investigating Regional Patterns of Childhood Obesity: New Nationwide ECHO Study Investigates Regional Patterns of Childhood Obesity
For policymakers, health care professionals, schools, and families to effectively curb rates of childhood obesity, we will need to better understand where this risk comes from and how it can be managed. Research has shown that social, cultural, and environmental factors can strongly influence a child’s risk of developing obesity, indicating that the burden of obesity may vary by geographic region and sociodemographic background.
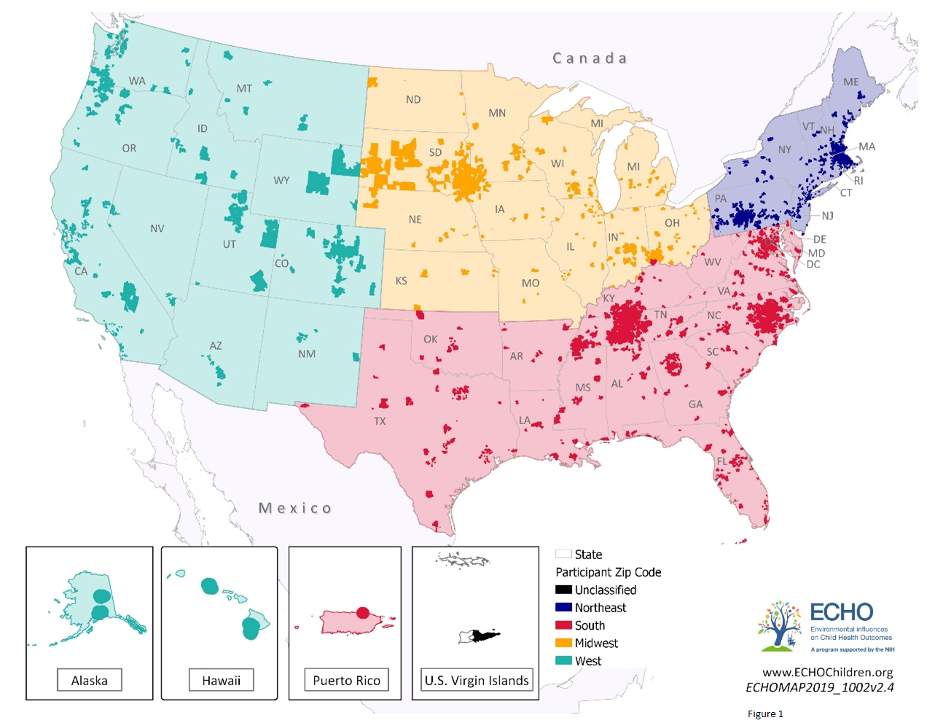
To develop a more complete understanding of how patterns of childhood obesity risk vary by geographic region, Traci Bekelman, PhD, MPH and Dana Dabelea, MD, PhD of the University of Colorado Anschutz Medical Campus led a team of ECHO researchers and conducted a nationwide study of over 14,000 children and teens from 25 ECHO cohorts across 50 states. Researchers divided the children into four regional categories—West, South, Northeast, and Midwest. The researchers used information about each child’s height and weight to calculate their body mass index (BMI), an approximate measure of body fat that is often used to assess obesity. They then compared BMI patterns for different sociodemographic groups and across all four U.S. regions.

The study, published in Obesity, found Black children in the Northeast, South, and Midwest and Hispanic white children in the South and West had higher BMIs on average than their non-Hispanic white counterparts.
The results of this ECHO study are an important first step toward identifying the regional and systemic policies and practices that contribute to childhood obesity risk. Understanding the sources of obesity in children can help doctors and policymakers design more effective prevention strategies to keep children healthy as they move into adulthood.
We sat down with Dr. Bekelman and Dr. Dabelea to discuss their recent publication and gain some additional background on their collaborative study with the ECHO Program. Together they provided comments about the significance of this study and the future of obesity research.
Investigator Insights
“In adults, there is a regional difference for burden in major chronic disease,” explained Dr. Dabelea. She said these health outcomes in adults can be traced to regional differences in the U.S., making it important to look at these variations in early childhood to understand health outcomes later in life.
“Part of the inspiration was to leverage the power of ECHO’s harmonized data and unique population size, which is especially important when looking at health disparities across different demographics and regions,” said Dr. Bekelman. Both investigators noted that such data do not exist for children, particularly for childhood obesity.
One factor the investigators examined was how a mother’s level of education is associated with child BMI. Childhood obesity is higher among children who live in households with a lower income. The study found that a lower level of formal education among mothers was associated with higher childhood BMI across all regions observed.
COVID-19 and Future Research on Obesity
Both investigators are leading a team of ECHO researchers to study how the social and economic disruption of the COVID-19 pandemic has affected children’s lifestyle behaviors. This research, which is part of the ECHO COVID-19 projects, funded by the NIH in summer 2020, includes analyzing lifestyle data that children provide during ECHO visits. While official results from this ECHO COVID-19 project are expected to be released in the fall, Dr. Dabelea said she expects the results to show changes in diet, physical activity, and screen time. The pair is also conducting qualitative interviews with parents to see if and why these lifestyle changes might be occurring.
Regarding future childhood obesity research, Drs. Bekelman and Dabelea want to further examine hypotheses surrounding childhood obesity outcomes and exposures. “Our latest study on investigating regional patterns of obesity didn’t necessarily test a hypothesis; it was a descriptive epidemiological study, which is designed to be hypothesis generating, not hypothesis testing,” said Dr. Dabelea. She noted that testing hypotheses on differences found in U.S. regions in terms of fast food restaurant density, accessibility to parks and playgrounds for exercise, school nutrition policies, and other exposures influencing childhood obesity outcomes also remain pertinent in understanding this health outcome.
Back to top
News You Can Use
We're Hiring!
The ECHO Program Office is seeking to hire a Health Scientist Administrator (Program Officer) GS-601-14. Please read the full announcement here, and share with anyone in your networks who may be interested. This position is open for application until September 29.
Conceptual Models for Implementing Solution-oriented Team Science in Large Research Consortia
In a new paper published in the Journal of Clinical and Translational Science, authors from NIH draw from lessons learned in ECHO to provide two conceptual models for guiding the design, implementation, and evaluation of large and complex research programs. These conceptual models can help programs map out—and continuously improve—the teams, tasks, tools, and workflows needed to operationalize their scientific goals.
ECHO Publication Examines Link Between Genetic Changes and Wheezing Patterns in Children
For many children, wheezing is an early indicator of childhood asthma. Many studies have investigated the different patterns of wheezing and their connection to asthma diagnosis, but there is little research around how different genetic variants associated with asthma are linked to these wheezing patterns. In order to fill this gap, Brian Hallmark, PhD and researchers from ECHO Children’s Respiratory and Environmental Workgroup (CREW) investigated the link between genetic variants and wheezing patterns in African American and European American children across the U.S. This was the first such study to include a sizable number of African Americans, which enabled the researchers to pinpoint certain genetic changes common to both race/ethnic groups.
The team compiled data on how often children in the study wheezed from birth to 11 using questionnaires and interviews with children and their parents. They also collected DNA samples from children and used those samples to identify nine different small genetic changes.
The researchers identified four different wheezing patterns among the children who participated in the study—infrequent, transient, late-onset, and persistent—and found that only two of the small genetic changes associated with asthma were linked with wheezing in both European American and African American children. One of these small genetic changes interrupts the production of a protein that may be important for protecting the body from a viral infection in the upper airways.
“Asthma is complicated, and susceptible children exposed to hazards such as viruses, allergens, and pollution have more risk of having episodes of wheeze in the preschool years,” said Dr. Hallmark. “The more we understand how asthma develops, the better we can identify and help children at risk and find ways to prevent asthma.”
The article, titled “Chromosome 17q12-21 Variants Are Associated with Multiple Wheezing Phenotypes in Childhood,” is published in the American Journal of Respiratory and Critical Care Medicine.
ECHO Publication Explores Best Practices for Conducting Clinical Trials with Indigenous Children
The US population includes nearly 7 million Indigenous people, including 5 million American Indian and Alaska Native (AI/AN) people and 1.5 million Native Hawaiian and other Pacific Island people. Compared to other demographic groups, Indigenous communities disproportionately experience structural barriers to health, such as household crowding, lack of plumbing and clean water, indoor air pollutants, and environmental contamination. These health disparities negatively impact Indigenous children through significantly higher rates of asthma, obesity, and respiratory infections, compared to the general pediatric population.
One of the goals of ECHO’s IDeA States Pediatric Clinical Trials Network (ISPCTN) is to address disparities in pediatric research by increasing representation of children from rural or underserved populations in clinical trials. Indigenous children are more likely than their peers in all other racial groups to live in these areas and are underrepresented in pediatric research. In a new paper out this month in the American Journal of Public Health, ISPCTN authors highlight best practices for conducting clinical trials with Indigenous children in the United States.
The authors provide guidance for conducting ethical and effective clinical trials with Indigenous children and highlight the challenges in enrolling Indigenous children in clinical trials. These include the burden on families of traveling to urban research centers, where trials typically occur, past research misconduct in Indigenous communities, and conflicts between Western scientific practices and Indigenous priorities.
Dr. Shaw and her co-authors also describe 3 best practices, with case examples, for conducting clinical trials with Indigenous communities—ensuring early and sustained community engagement, building Indigenous research capacity, and supporting community oversight and ownership of research. They contend that “improving health outcomes in this pediatric population of more than 2 million children requires increasing their enrollment in clinical trials to ensure the development of effective, population-based interventions that can be successfully implemented.”
You can read the full paper here.
Back to top
ECHO Study Investigates Innovative Way to Assess Simultaneous Exposure to Many Chemicals in Pregnant Women
Pregnant women may be exposed to a variety of chemicals that could pose a risk to them or their baby, including endocrine disrupting chemicals (EDCs) that can interrupt growth and development. The effects of EDCs are often studied individually, but mothers tend to be exposed to a combination of chemicals during their pregnancy. To better investigate the effects of chemical mixtures, ECHO researcher John Pearce, PhD of the Medical University of South Carolina and his team used a novel technique to identify different maternal exposure patterns and investigate their associations with infant birth weight.
The researchers collected blood samples and infant birth weight from 600 women. The team used an exposure continuum mapping (ECM) framework to identify a wide variety of chemical exposure patterns that mothers were exposed to and examined how those patterns affected the birth weight of their children.
Exposure profiles containing higher levels of polybrominated diphenyl ethers (PBDEs), found in flame retardants, were linked with lower infant birth weights. On the other hand, exposure profiles containing higher levels of polychlorinated biphenyls (PCBs), found in industrial and commercial products, and perfluoroalkyl (PFAS) substances, found in some food packaging and drinking water, were linked with higher infant birth weights.
“ECM provides a promising framework for supporting studies of other exposure mixtures,” said Dr. Pearce. “Moving forward, our team will explore associations between exposure mixtures and other child health outcomes, with particular interest on obesity.”
The article, titled “Exploring associations between prenatal exposure to multiple endocrine disruptors and birth weight with exposure continuum mapping,” is published in Environmental Research.
Back to top![]()
ECHO Discovery
ECHO Discovery is a monthly webinar series with educational presentations for the ECHO community, stakeholders, and the public.
Upcoming October ECHO Discovery

Speaker:
Learn about the October ECHO Discovery presentation.
August ECHO Discovery
Understanding Health Disparities: What You Don’t Know Can Hurt You

On August 11, Nathan Stinson, Jr., PhD, MD, MPH of the NIH National Institute on Minority Health and Health Disparities (NIMHD) gave an ECHO Discovery presentation on understanding health disparities among minorities and underserved populations.
Minority Health Research
Throughout his presentation, Dr. Stinson discussed the importance of minority health research in understanding why different minority populations experience specific health outcomes compared to non-minority populations. “Race and ethnic minorities share a social disadvantage based in part on being subjected to discrimination as a common theme,” he said. Dr. Stinson said that a disparity can be defined as a health outcome that is worse in these populations compared to a reference group.
Dr. Stinson discussed the social determinants of health that can lead to these disparities, such as age, gender identity, race/ethnicity, sexual orientation, religion, disability status, socioeconomic status, and more. These factors can affect how these populations can access housing, employment, economic opportunities, and health care. Following the onset of the COVID-19 pandemic, Dr. Stinson said racial and ethnic minority populations have been disproportionately affected and have had higher chances of becoming infected with the SARS-CoV-2 virus and experiencing economic hardships.
Research Needed to Reduce Health Disparities
To address health disparities among minority populations, there are many things that need to be done to manage the discrimination that leads to this inadequate health.
Dr. Stinson explained that it is important to recognize the value of maintaining health and educating groups on healthy habits, not just of health care itself. Additionally, he said that policy makers and public health officials should shift health care models to include population health by measuring social determinants of health, create better access to healthy foods and safe places, provide community health resources, and recognize structural and interpersonal discrimination.
![]()
July ECHO Discovery
Community Engagement and Report Back: the Story of PROTECT-ECHO in Puerto Rico

On July 14, Carmen M. Vélez Vega, PhD, MSW of the University of Puerto Rico gave an ECHO Discovery presentation where she discussed the PROTECT-ECHO project in Puerto Rico. PROTECT (Puerto Rico Testsite for Exploring Contamination Threats) began in 2010 with the goal of understanding why Puerto Rico was ranked third in the world for highest preterm births.
Dr. Vélez Vega’s presentation covered how her team implemented community engagement and a report back system for the success of the project.
“The PROTECT Center studies exposures to environmental contamination in Puerto Rico and its contribution to preterm births,” Dr. Vélez Vega said. Investigators took samples from pregnant women to look at the health effects of environmental contaminants such as phthalates and chlorinated solvents in relation to high preterm birth rates. The cohort became part of the ECHO Program in 2017.
The Significance of Participant Engagement
To ensure high participant engagement, the project team implemented a report back system via a project-specific smartphone application. Throughout sample collection and participation, there was an emphasis on cultural identity and getting an accurate snapshot of typical foods eaten and household cleaning supplies used.
Participants utilized the mobile phone app to create personal profiles where they could view their results and analyses, along with recommendations on how to reduce environmental and chemical exposures. Women were also able to share their experiences with each other, and play an active role in providing feedback to investigators. Dr. Vélez Vega noted the high level of participant interest is because pregnant women want to contribute to science and understand why premature births are happening to them and their families.
Community Engagement and the COVID-19 Response
The main vehicle of interaction with community stakeholders and participants throughout PROTECT-ECHO is the Community Engagement Core (CEC). This group utilizes participation and engagement resources to gather feedback and disseminate information to stakeholders throughout the community.
The CEC was extremely helpful to investigators following the onset of the COVID-19 pandemic, as well as during other events such as earthquakes, hurricanes, Zika virus outbreaks, and the evolving demographics of Puerto Rico. Since computer access is limited due to socioeconomic factors, natural disasters, and health events, call centers were set up for investigators to follow up with participants. The project team also utilized outreach methods such as text messaging, and provided educational materials to participants via email and social media.
Dr. Vélez Vega and the project team are currently working on the PROTECT Responde Campaign to feature videos, educational materials, and resources on environmental contaminants and health impacts during COVID-19 via social media. This will allow participants and community members in Puerto Rico to learn more about how to keep themselves healthy throughout pregnancy and potentially reduce rates of preterm birth for themselves and family members.
Learn More about ECHO Discovery
Back to top

Subscribe to receive a copy of the ECHO Connector newsletter through email.
Questions?
Contact the ECHO Program Office.